
The Stancounty.Com website has been translated for your convenience using translation software powered by Google Translate. *Note: Prescription must include patient name, birth date, name of formula, medical diagnosis, amount needed per day, duration, and signature of healthcare provider.

This program connects children with publicly funded health care and insurance, which expedites enrollment of income eligible children into Medi-Cal if they are not already enrolled. WIC Nutritionist will instruct participant to take a complete RX to a different pharmacy if initial pharmacy is unwilling to investigate and resolve the reason for the denial.įor Medical Coverage: Refer patient to C4Yourself to apply for Medi-Cal coverage.įor Temporary Medical Coverage: Refer patient to CHDP Gateway Program at 1-80.

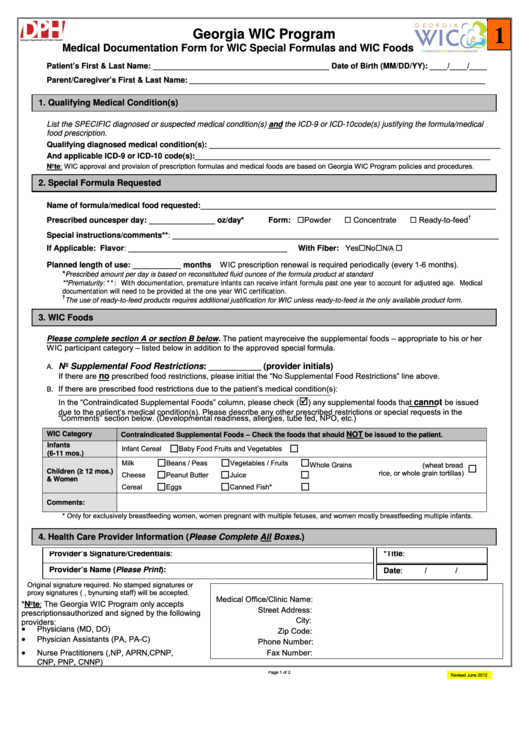
Once denial is verified WIC will issue formula. Verbal denial will be verified by a WIC Nutritionist by calling the pharmacy. If the therapeutic formula is denied, the patient should return to their WIC site with verbal or written denial from the Pharmacist stating the reason for denial. Physician should tell patient to take Rx to pharmacy for filling. The Physician should provide patient with a complete prescription* written on office letterhead or script pad. Local WIC agency may provide therapeutic formula if WIC therapeutic issuance requirements are met, and until the appeal process is successful.įull Scope Medi-Cal (a.k.a. If the patient is experiencing difficulty obtaining plan coverage, they should call the Medi-Cal Managed Care Ombudsman at 1-88 to resolve any problems and appeal the denial. The phone number is on the back of their benefits card. The patient should call membership services for the plan if they need help. Physician needs to provide complete Rx for formula and tell patient to take to a pharmacy that contracts with the specific Medical Managed Care plan. For specific MMC policy information on therapeutic formula provision go to MMCD Policy Letter. Medi-Cal Managed Care Plans (MMC) are required to provide medically necessary formulas. Physician must submit a request for prior authorization to the health plan. Medi-Cal Managed Care Plan (Health Plan of San Joaquin, or HealthNet): Local WIC agency may provide therapeutic formula if WIC therapeutic issuance requirements are met. If the health plan denies the formula, patient should take the complete prescription to their WIC site for Nutritionist evaluation. Physician must submit the required paperwork requesting the formula to the health plan. Therapeutic Formula Coverage Options Private or Military Insurance: WIC will require a prescription* as well as a letter of denial from the health plan or Medi-Cal.Ĭhoose the formula that is right for your patient. Should your patient be denied coverage by Medi-Cal or other health insurance, WIC may provide the therapeutic formula. WIC can provide formula temporarily while coverage is pending. As part of the patient’s treatment plan, therapeutic formulas should be covered by the health plan when the clinician provides adequate medical justification. If one of WIC’s contract formulas is not appropriate for your patients, there may be a medical condition warranting a therapeutic formula. Use the appropriate WIC referral form.Ģ.Ĝomplete the form and ensure it includes the patient’s labs (hemoglobin and hematocrit, lead levels and height and weight) and is dated and signed. Pediatric Referral Use for therapeutic formula referralġ. WIC can assist with nutrition education, breastfeeding support and supplemental food. There are many reasons to refer your patients to WIC.

Welcome to Online Education! Once you’ve created an account you can start your online class.
#Wic formulas password
NOTE: Be sure to create a simple, easy-to-remember Username and Password for future access to your online education account


 0 kommentar(er)
0 kommentar(er)
